William H. Calvin and George A. Ojemann, Inside the Brain: Mapping the Cortex, Exploring the Neuron (New American Library, 1980), chapter 8. See also http://WilliamCalvin.com/ Bk1/bk1ch8.htm. |
William H. Calvin
University of Washington |
|
8 Seizures: Electrical Storms of the Brain |
©1980 by William H. Calvin and George A. Ojemann |
Neil is moving around restlessly, not an uncommon problem after four hours on the operating table, but the anesthesiologist reports that Neil is making fumbling movements with both hands. "Neil, how are you feeling?" asks the neurosurgeon. "Feel funny. . . . I see that man walking his dog again. . . . He's getting bigger, and he's almost to the middle." "Neil? What's happening now?" There is no response from Neil. The fumbling movements of his hands become more pronounced, and he tries to move around but is restrained by the anesthesiologist and the circulating nurse. After a minute, Neil quiets down but still does not respond to questions. The neurosurgeon takes the opportunity to describe what is happening to those medical students watching from the gallery. "What you just saw was one of Neil's typical seizures. He often has this hallucination, the man walking his dog. That's the 'aura' which heralds his seizures. He knows that when the man and dog reach the middle of the picture, he is going to lose consciousness and not remember anything afterward. It's called a psychomotor seizure, and it only occasionally progresses to become the typical major motor seizure, with all of the rhythmic twitching of arms and legs." "Neil, can you hear me?" the neurosurgeon asks repeatedly for several minutes. "Wha . . . What'd you say?" "Neil, tell me what happened." "Don't know . . . guess I had a seizure, didn't I." "Did you hear me talking about you just now?" "Don't remember." "Do you remember seeing slides that you named for me?" "Yes, I think so. . . ." "When was that, Neil?" "You brought that slide projector to my room last night, I remember now." "What have we been doing this morning, Neil?" "You gave me those shots with the hypodermic needle. . . . And then, I remember now, you showed me those slides again," "Did you see anything unusual, Neil?" "That's right, I saw that man walking his dog again. He got all of the way to the middle of the picture this time, I remember him getting all of the way to the middle." "All right, Neil. You did have one of your little seizures. Everything is going fine, so just rest for a while."
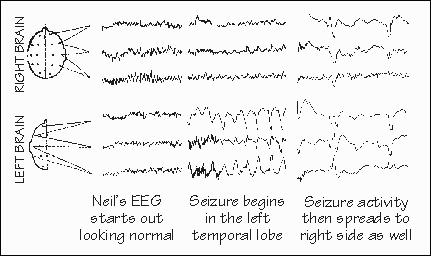
Seizures such as Neil's often begin in one spot in the brain, where the damaged nerve cells are located. This site is called the focus. Then the seizures spread to surrounding, more normal brain. The first symptoms of the seizure, from the disturbed function of the brain in the focus, are often called the seizure "aura." Since seizures often start in the same spot, these aurae are frequently the same from one seizure to another. Not everyone with focal epilepsy has an aura. But many patients with foci in the temporal lobe have aurae such as Neil's: either a hallucination (a sensation of something that is not there) or an illusion (a distortion of something that is). Hallucinations may be visual, such as Neil's picture of a man and a dog at the start of each seizure. Another patient may see a bucolic farm scene at the start of each of his spells; other patients may hear voices, or music, or smell something (usually unpleasant). Very occasionally, an aura will consist of a specific event from the patient's past, a hallucination whose implications for our knowledge about human memory have been discussed. One common illusion at the beginning of a temporal-lobe seizure is fear, or feelings of unusual familiarity ("I've been here before," known as déjà vu). Objects may seem unusually far or near. One illusion that these patients are often reluctant to report involves alterations in the apparent size of things; they are afraid that others might think them crazy if they admit that they sometimes see giants and little people. Spread of the seizure into wider areas of the temporal lobe is associated with automatic movements: walking, fumbling with things, muttering a few words. When the seizure extends to the hippocampus, there is a loss of memory for recent events. But during such a "psychomotor" seizure, the patient seldom does anything elaborately purposeful or planned, such as cooking a meal, stealing a car, or (as in a popular novel) destroying a computer center. He is unlikely to harm another person, except by accident. (The Terminal Man was both epileptic and psychotic.) "Temporary insanity" defenses are still sometimes used in criminal trials, the defendant claiming no memory for robbing the bank and blaming it all on a psychomotor seizure, even though there is almost no medical evidence that this ever happens. Neil's seizure in the OR was one of his "little" seizures. He sometimes has a little seizure of his usual type, followed by a major motor seizure. This "big" seizure, which is what most people think seizures consist of, involves rhythmic jerking of both arms and legs; indeed the whole body seems to go through a sequence of stiffness followed by jerking, and then a relaxed period of unconsciousness. Such seizures seem to involve the simultaneous induction of abnormal electrical activity in widespread areas of both sides of the brain. The electrical "batteries" upon which nerve cells operate are severely discharged, and the unconscious period corresponds in part to' the time needed for the battery-charging mechanisms (actually metabolic pumps, moving sodium and potassium across the membrane of the nerve cell) to reestablish normal voltages. Ncil, reading about this earlier, observed that it sounded like a computer center "coming back up on line" after a power failure. How do anticonvulsant drugs. prevent seizures? Mostly, they seem to prevent the spread of seizures within the brain; there is little evidence that they get at the root of the matter and quiet down the primary pathology, in the way that levodopa is thought to work in Parkinson's disease. One anticonvulsant, sodium valproate, is thought to increase the stockpile of the neurotransmitter GABA in the brain. This neurotransmittcr acts in an inhibitory manncr, decreasing the electrical activity in downstream neurons. Thus the anticonvulsant might be acting by preventing the runaway conditions which occur when inhibitory neurotransmitter supplies become exhausted: a little seizure might still get started, but surrounding neurons would be more resistant to being fatigued into runaway activity. The physiologic mechanisms that allow little seizures to get bigger by "taking over" normal neurons are reasonably well known, but why that spread occurs only occasionally, rather than all the time, is much less clear. Certain things seem to increase the likelihood of seizure spread in a particular patient; drowsiness and emotional stress are two fairly common ones. Some patients find little "tricks" that seem to prevent seizure spread. One patient found that thinking about something else the moment he detected the seizure would stop it. In another patient, touching an arm or the face may stop the spread of the seizure. A more elaborate strategy to stop seizure spread is to let the patient learn to alter his own EEG by blofeedback. Usually this involves feeding back a signal to the patient that tells him how much of his EEG is in a particular frequency range. The patient then tries to find ways of changing that signal, usually shifting the EEG to higher frequencies. Jn an occasional patient, seizure rates decrease. But with seizures influenced by so many things, it requires a very carefully designed study to be sure that the treatment is really effective-whether it is actually the biofeedback, or the new drug, or the new operation that has decreased the seizures. Even bringing a patient into a hospital and doing nothing else often reduces seizure rate and severity, sometimes stopping seizures altogether for a while. This is the reason that controls are so essential to Studies of treatments for seizures. In such rigorous studies, a number of old standbys and some widely publicized new treatments for epilepsy don't seem to do anything specific. What would cause the rapid spread of Neil's seizure out of the left temporal lobe to involve many regions of both sides of the brain at once? The spread can be so sudden that the EEG experts often speak about "the wrong switch having been pushed," and there has been much speculation about the brain mechanisms involved. The seizure does not simply spread like a wave across the surface of the brain, one region involving its neighbor in the manner of a forest fire. It appears that the very mechanisms which the normal brain uses. to control levels . of arousal, to control sleep and wakefulness, have become involved in the seizure. These mechanisms are collectively called the reticular activating system and are known from several decades of animal experiments to reside deep in the core of the brain. They have widespread connections to all parts of the brain on both sides, like a manager with a finger in every pie. The reticular activating system has two component parts. One part regulates overall arousal and the various aspects of the sleep-wakefulness cycle; another provides selective attention. The arousal part of the system, located in the upper part of, the brain stem, acts like an amplifier placed in parallel with sensory inputs. When turned on, this amplifier takes those sensations and boosts them in order to "wake up" the cerebral cortex. A seizure spreading to this amplifier could rapidly spread to the whole cortex. A small seizure from anywhere can spread into this amplifier. Should the seizure start in a piece of -brain that has an easily detectable function, the first sign of the seizure will be a change in that function: a jerk of the hand if the seizure starts in motor strip, or a hallucination if it starts in temporal lobe; only after that warning will the rest of the brain become suddenly involved in the seizure. For many brain areas, however, there is no easily detectable function (no "local sign," as the neurologists call it) to serve as a warning.' The first indication of a seizure may only come after it has spread into the activating system: the stiffening and jerks of a fullblown seizure involving many regions of both sides of the brain. These "big seizures 11 are called by their French name, "grand mal. " Another common seizure also seems to involve the reticular activating sysem. In these seizures, the reticular activating system "amplifier" seems to be switched off briefly, rather than excessively activated as in big seizures. So the symptom of these seizures is a brief interruption of consciousness. This type of little seizure is, called "petit mal. " This seizure type typically comes on in early childhood, often changing its nature, indeed even sometimes disappearing as the child reaches puberty. Of all the seizure types, it is one of the few in which a family history of epilepsy is fairly common. Patty's third-grade classwork had been getting worse. Her teacher and her parents considered her to be a normal eight-year-old, although given to "daydreaming" and "not paying attention." On spelling tests, there were gaps in the test paper, where she failed to write down two or three words. Patty said that she just didn't hear them. The words which she did write down were spelled correctly most of the time. Her physician was suspicious and sent her to a neurologist. As Patty talked, the neurologist noticed that she would stare fixedly for brief moments. An EEG later confirmed that these lapses were from brief seizures, involving both sides of the brain at the same time, causing brief periods where Patty was simply out of touch with the world around her, just as if a switch had been turned off and then back on again. Patty was started on the anticonvulsant drug sodium valproate when it was released for use in the U.S. by the F.D.A., some years after its introduction in Europe. That drug has completely controlled her seizures and her schoolwork is finally back to normal.' |
 Continue to CHAPTER 9
Continue to CHAPTER 9
Notes and
References for this chapter Copyright ©1980 by |