|
Conversations with Neil’s Brain The Neural Nature of Thought & Language Copyright 1994 by William H. Calvin and George A. Ojemann. You may download this for personal reading but may not redistribute or archive without permission (exception: teachers should feel free to print out a chapter and photocopy it for students). William H. Calvin, Ph.D., is a neurophysiologist on the faculty of the Department of Psychiatry and Behavioral Sciences, University of Washington. George A. Ojemann, M.D., is a neurosurgeon and neurophysiologist on the faculty of the Department of Neurological Surgery, University of Washington. |
|
When Things Go Wrong with Thought and Mood
TRUSTING WHAT YOU SEE AND HEAR isn’t just a matter of judging the reliability of
other people. For some patients, “Did it really happen?” refers to the sensation
itself — was it real or imagined? I hadn’t wanted to bring up Neil’s
hallucinations so soon after we discussed the important issues of muffins versus scones, latté
versus cappuccino — but Neil reminded me of that odor of burning rubber that sometimes
preceded his seizures. |
|
INHERITANCE HAS A LOT TO DO with both schizophrenia and mood disorders. A major
way to sort out environmental influences from biological ones is through the study of twins
separated at birth by adoption into separate homes. If one identical twin has schizophrenia,
there’s about a 50 percent chance that, when the other twin is located, he too will be
schizophrenic. For fraternal twins, the chances are only those of siblings in general —
about one in six. The incidence of schizophrenia in the adoptive parents has little influence. The
data is similar, though not as strong, for mood disorders. However, a genetic predisposition does not seem to be the only factor that accounts for these disorders. Even with the identical genetic makeups of identical twins, about half of the identical twins of schizophrenics never develop the disease. So the environment, the accidents of upbringing and exposure to viruses, made the difference between having the genetic predisposition and actually coming down with the disease. 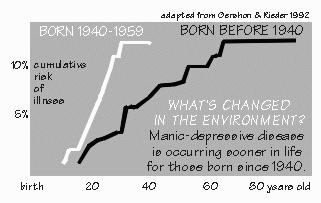 [FIGURE 49 Manic-depressives born before or after 1940] The importance of some environmental factor in these illnesses is particularly apparent for mood disorders, because something seems to have changed after about 1940. Most of the people who are going to get a manic-depressive disorder will have gotten it by age 30, if they were born after 1940. But for people who were born before 1940, it took several decades more to develop. Relatives of patients with mood disorders born after 1940 are also more likely to have the illness than relatives born before that date. The environmental factor is unknown. One way of looking at these disorders is that they change the way the brain responds to novel environmental cues and are thus less evident in a stable environment. “Which our current times certainly are not,” Neil added. The first clinical episode, in both the thought and the mood disorders, often occurs in adolescence. It may appear suddenly, seemingly triggered by an inconsequential event. Both thought and mood disorders tend to wax and wane during life, with episodes becoming more frequent as the patient gets older. Schizophrenics usually do not recover completely between episodes, while those with mood disorders often function entirely normally in the intervals between exacerbations. However, patients with either type of illness can lead productive lives. One of these days, we’ll consider them organic psychiatric disorders but, despite extensive research, the brain abnormalities in both disorders are not completely known. In each type, abnormalities seem to be present in multiple brain areas, suggesting that the defect is in a broadly-based brain system — such as those lawn-sprinkler systems using serotonin and norepi coming up from the brain stem — rather than a specific anatomic area. Moreover, the most effective drug treatments for each disorder tend to affect systems of nerve cells that use particular transmitters. For mood disorders, it’s the neurons that use norepinephrine, dopamine, and serotonin (collectively called the monoamines) as neurotransmitters. For schizophrenia, the effective drugs relate to neurons that use dopamine and glutamate. Or maybe the problem is in neurons downstream from them. There are many different postsynaptic receptor types for each of the neurotransmitters, such as those ordinary and NMDA receptors for glutamate. The same key fits several locks, in other words. And only some of the receptor types seem to be involved in the disease. In mood disorders, effective drug therapies seem to alter a class of receptors that are linked to a specific substance in the cell’s cyclic adenosine monophosphate, decreasing the amounts of that intracellular “second messenger.” In schizophrenia, the balance between nerve cells using dopamine as a transmitter and those using glutamate may be the important factor, with excessive dopamine levels or inadequate glutamate levels the likely problem. Although these abnormalities in systems of nerve cells using specific transmitters have effects throughout the brain, different parts seem to be more affected in one type of disorder. Temporal lobe abnormalities seem to particularly characterize schizophrenia. More patients have both schizophrenia and temporal lobe epilepsy than would be expected by chance, although most patients with temporal lobe epilepsy are otherwise normal. “So you can operate on the temporal lobe and cure schizophrenia, just as with my type of epilepsy?” Unfortunately, no. Curing the epilepsy in these patients doesn’t help schizophrenic symptoms if they are already present, nor prevent their later appearance. One investigator, however, reported that schizophrenia is more likely in patients whose epilepsy was associated with a specific anatomic change in the temporal lobe, known as “hamartomas.” They are little pockets of nerve cells buried in the white matter where they don’t belong, evidently because of a developmental misstep during gestation. That finding hasn’t been confirmed, but magnetic resonance imaging of patients with schizophrenia alone has shown changes in temporal lobe — for example, a 20 percent loss in gray matter volume and atrophy of the hippocampus. Sometimes the hallucinations associated with small seizures in the temporal lobe have characteristics suggestive of schizophrenic thought, especially paranoia. George told me about one such patient of his, who had a paranoid experience upon stimulation of the surface of the temporal lobe. “I thought you said they didn’t operate for paranoia?” Not by itself — this guy had a brain tumor. He had been referred to a psychiatrist because of increasing suspiciousness and unusual thoughts over the past few months. He even occasionally heard voices talking about him. The psychiatrist thought he “looked organic” and so ordered an MRI. It showed a tumor in the frontal lobe in a very awkward place: close to the motor strip and language areas. So that operation involved stimulation mapping with the patient awake, similar to the mapping that is needed during epilepsy operations. The operation for this tumor was going very smoothly. The patient had cooperated completely with all the testing, and George had identified the face motor area, as well as the frontal (Broca) language area. The tumor was just between them. Then George applied the stimulating current to the temporal lobe, just below the motor and speech areas. And the patient unexpectedly said, “I hear people outside talking about me.” George chatted with the patient for a moment and went on to test more of the frontal lobe. The patient performed the tests with no other comment — until the temporal lobe site was stimulated again without warning. The patient immediately asked, “Is the radio on? I hear something on it about me.” Later the temporal site was stimulated a third time, and again he volunteered that he heard voices saying things about him. “I remember that you said something about Penfield’s patients, that they often reported unidentified voices offstage. If that’s the most common kind of experiential response, suppose that the temporal lobe is the scene of the crime in paranoia?” That’s not clear yet. The blood flow to the tip of the temporal lobe does increase in studies of anticipatory anxiety. Usually anxiety doesn’t go away when one temporal tip is removed in epileptics — although, if there is any consistent personality change after that operation, it is in the direction of being less anxious. Actually, contrary to popular belief, hallucinations were not part of the original definition of schizophrenia. Eugen Bleuler, a Swiss psychiatrist of Freud’s generation, coined the term. He thought that hallucinations, because they were so often seen in manic-depressive illness, were secondary to his “four As” of schizophrenia that were taught to generations of psychiatrists: affective blunting, association disturbances, autism, and ambivalence (by which he meant indecisiveness). But these days, the criteria for schizophrenia emphasize prominent hallucinations and bizarre delusions. |
|
DELUSIONS are also a thought disorder, as opposed to a disorder of perception. Together,
hallucinations and delusions are known as psychotic symptoms. “And the psychotic symptoms are most commonly seen in schizophrenics?” While they’re seen in all schizophrenics, it’s actually the people with mood disorders who have more psychotic symptoms. That’s why it’s important to distinguish between the psychoses — the psychiatric diagnoses, such as manic-depressive illness — and the psychotic symptoms. Only half of the manics and a fifth of the depressed have psychotic symptoms — but mood disorder patients are many times more common in the population than are schizophrenic patients. Needless to say, it sometimes confuses the diagnosis. In any event, if anybody you know has a psychosis, it’s more likely to be from a mood disorder than from a thought disorder. There are also people who primarily have delusions, but none of the functional deterioration and bizarre delusions that characterize schizophrenia or the mood swings that characterize the other major source of delusions. The delusional-disorder patients mostly have delusions — but occasional hallucinations as well. What they don’t have is the gradual deterioration seen in schizophrenia, which makes the disorder especially devastating. Delusions are firmly held beliefs that are both untrue and contrary to what the patient’s culture provides in the way of explanatory metaphors. Thus magical thinking might be delusional in a college kid from the white suburbs, but it may be just cultural if the patient is a ghetto kid whose parents are from Haiti. The common delusional-disorder patients are the paranoids, the pathologically jealous, the persons with grandiose delusions about their special relationship to a celebrity such as John Lennon, the people who think they’re the devil and are condemned to burn in hell. Some have somatic delusions — maybe they are absolutely sure that some part of their body is shrinking over time. But people with delusional disorder aren’t disorganized the way schizophrenics tend to become. They have well-preserved personalities and they have rationalized their symptoms to the point that they have an answer for everything odd they experience. They seldom need hospitalization. And they can usually can stay employed. “Right. As leader of the Third Reich. Or of the Branch Davidians.” Yep. Hitler, David Koresh — they had good sales and leadership skills, in addition to delusions. The delusional can be so sure of themselves, so certain they are special, that they can attract followers who will do almost anything. And with their occasional hallucinations, the delusional may have some interesting visions to report — which, of course, they weave into their well-rationalized explanations of conspiracies afoot and revelations to come. “So what defines a schizophrenic, then? Their hallucinations and delusions are simply more bizarre?” Their delusions are indeed more bizarre, such as thoughts being broadcast into their heads or being controlled by men from Mars. But what defines any psychiatric disorder is the combination of symptoms and how long they last, not one particular symptom. It can be terribly confusing on slight acquaintance, as you focus on one symptom, see it in yourself perhaps, and worry. Just think of all those middle-aged people who worry that their “memory problems” constitute a slippery slope into Alzheimer’s dementia — not realizing that the folks who are alert and lively at 92 have also been complaining about their difficulty remembering people’s names for the last 45 years. The combination of symptoms that provide the diagnostic criteria for schizophrenia include prominent hallucinations and bizarre delusions for some period of time, not just as a drug reaction. The diagnosis assumes you’ve ruled out a mood disorder first. And the diagnostic criteria emphasize a deterioration of functioning — in work, social relations, self-care - that isn’t seen in the other thought disorders. Both schizophrenia and mood disorders show evidence of decreased activity in frontal lobes and abnormal function of the system for directed attention. Mood disorders also show abnormal function in the hypothalamus, particularly in the regulation of the hormones involved in responses to stress. |
|
THE DEVELOPMENT OF DRUGS altering transmitter levels has allowed many patients with
these conditions to function normally, or nearly so. However, a few patients do not respond to
drug therapy. In the 1920s, physicians observed that mental patients who also had seizures were,
paradoxically, better after a grand mal seizure, especially in their mood. This was the basis for
electroconvulsive therapy for depression, a treatment valuable in depressed patients not
responding to drugs, and which also seems to produce the same changes in neurotransmitter
receptors as do many of the effective drugs. Unfortunately, there remain a few patients with
severe depression whose symptoms persist despite drugs or electroconvulsive therapy. “What do you do for them? Surgery?” That’s an option. Psychosurgery is still alive and well after fifty years, although one would think, from popular beliefs — even among some psychologists, who should know better — that it was some sort of discredited mutilation from a mad-scientist age of psychiatry and neurosurgery. In the mid-1970s, the critics of psychosurgery helped persuade the U.S. Congress to establish the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. And to charge it, among other things, with evaluating psychosurgery. Needless to say, prominent critics of psychosurgery were represented on the commission. But when the commission issued its report in 1976, it turned out to be surprisingly favorable, concluding that the operations were useful in selected cases, provided that the patient is competent to give informed consent. It concluded that legislation wasn’t needed after all, that the regulation of psychosurgery could be left to the medical profession. Which goes to show that people shouldn’t get their medical information from novelists trying to create dramatic stories about Orwellian nurses dealing with troublemakers. “So it’s still an option for severe depression?” At least the kind that doesn’t respond to drugs and induced seizures. Modern versions of psychosurgery also help with obsessions and phobias, and it seems to have helped some schizophrenics. But the typical psychosurgery patient and typical brain lesion created is illustrated by someone like Edmund. He was an honor student in his final two years of high school. Nobody noticed anything wrong until he tried to kill himself — except, of course, Edmund himself, who had started noticing something wrong months earlier. Schoolwork wasn’t worth doing. Tennis wasn’t fun any more — he dropped out of that with an excuse about an injured knee. He didn’t have enough energy for anything. He felt he wasn’t “good enough” for his girlfriend; he saw her less and less. By the time he took all the sleeping pills, he was sure that life wasn’t worth living. Edmund’s psychiatrist started him on one of the newer antidepressant drugs as soon as he recovered from the overdose. That usually works, but for Edmund it didn’t — he just felt sleepier. There were therapy sessions with his parents, with his brother and sister, but Edmund continued to feel that he wasn’t “worthy” of them. Eventually, every possible drug having been tried without success, the psychiatrists recommended a series of electroshock treatments to induce seizures. These usually help, but Edmund was again the exception — he continued to feel that the only way to get rid of that awful blackness, the pain and unworthiness, was to die. While being walked around the hospital grounds, he broke away and jumped in front of a speeding car. Luckily, he got out of that with just a broken leg, and while he recuperated, there were more therapy sessions, more drugs, more electroshock. Still, nothing helped. He still felt empty and rotten inside, wanting to die. Now if our Edmund had lived in Great Britain, the next step would have been referral to a specialty center where psychosurgery is done. Several British centers have reported extensively on their experience with operations that destroy a small region on the inner face of the frontal lobe. This provides complete relief from depression in about half of the patients like Edmund; another third of the patients improve, although they do not get complete relief. In the British experience, the improvement lasts for five years or longer, with side effects in less than 2 percent of the cases. “Are any of the drugs for depression better than that?” asked Neil. No. Such modern psychosurgery is certainly an effective treatment for that small group of severely depressed patients like Edmund, who prove, for unknown reasons, to be unresponsive to drugs and electroshock. Despite this favorable British experience with modern psychosurgery, Edmund would probably not be treated with such an operation in the United States — even though there would seem to be no other options except waiting, with its hazard of suicide. “But why not treat them?” Because there are still too many people who would question the judgment of the clinicians involved and say that “everyone knows” that psychosurgery is “bad.” Nonetheless, the operation does get performed in the United States, but there are still many remaining pockets of ignorance-but-strong-opinion. The history of prefrontal lobotomies has a great deal to do with political controversy over modern psychosurgical operations. The original operation was also controversial in its day, even though it too marked a major advance for the treatment of the mentally ill and reduced the mortality from suicide. Cutting some of the connections in the white matter running between the front of the frontal lobe (“prefrontal”) and the rest of the chimpanzee brain was associated with more docility and placidity. These results were presented by the American neurophysiologist John Fulton at an international physiological meeting in 1935, where they came to the attention of an inventive Portuguese neurologist, Egas Moniz. So Moniz tried the same thing in humans. This innovation had many effects. The Moniz medical practice was disrupted by demonstrators opposed to psychosurgery. But, for the first time, a treatment was available that allowed some of the severely mentally ill to leave the asylum and return to society. Patients with depression, phobia, and obsessions were helped the most, patients with schizophrenia not as reliably. Indeed, the prefrontal lobotomy was so highly regarded that, in 1949, Moniz (but not Fulton) won the Nobel Prize for Physiology or Medicine. The medical profession soon recognized that this treatment was imperfect. Although the patients could leave the asylum, they often demonstrated some personality changes. Like George’s patient with the big tumor pressing on the inner sides of both frontal lobes, some lobotomized patients were uninterested in their surroundings, as well as unconcerned about the effects of their behavior on others. About this time, a French naval surgeon by the name of Laborit made an important discovery in the course of using chlorpromazine to treat sailors for worm infections. He noticed that his schizophrenic sailors with worm infections not only lost their worms but that the drug had a side effect: it calmed the mentally disturbed sailors. Now there was an alternative to psychosurgery, and many different drugs affecting dopamine receptors were tried. In animal research, it became apparent that the better a drug bound to the D2 version of the dopamine postsynaptic receptor, the more effective it was therapeutically in schizophrenics. Effectiveness had no relationship to binding to the D1 receptor type. 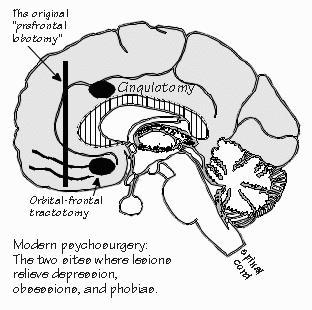 Schizophrenia wasn’t the strong suit for psychosurgery, in any event. And there were still lots of severe cases of depression, obsession, and phobia — so the psychosurgery operation was refined. Essentially, a much smaller lesion works just as well as the earlier ones but has many fewer side effects. In the modern operation, only selected areas are destroyed by using a small probe inserted through a small hole, in exactly the same way as the thalamotomies for Parkinsonism are done — just in a different place. The areas destroyed are on the inner face of the frontal lobe, usually on both left and right sides. In one operation, called a cingulotomy, a portion of the cortex just above the front end of the corpus callosum is destroyed. In the other effective operation, some white matter at the base of the frontal lobes is destroyed instead. In these modern operations, the change to an “uninterested” personality does not occur. And just as in the original operation, there is great improvement in the symptoms of depression, phobias, and obsessions, with schizophrenia not helped as much. These behavioral improvements occur only if the correct location is destroyed, not if the lesion is made nearby. There seems to be something specific about that portion of the brain for these mental disorders, especially depression, suggesting that the original operation destroyed far more brain tissue than was needed to get the desired relief. That specificity is very important, as one part of the debate over frontal lobotomy was how specific the treatment was. “Specific? How so?” Both foot amputations and insulin injections are treatments for diabetes, but only the latter is specific to the disease process. Physicians had worried, quite reasonably, that psychosurgery wasn’t specific enough. “So why all the fuss about lobotomies? Is it just a question of bad press?” The debate over psychosurgery was clouded by the failure of critics to distinguish between the modern operations, with their more specific criteria for operating on a patient and their infrequent side effects on personality, with the original Moniz operation, which made a much larger cut in the white matter and had the unfortunate side effects. That’s like criticizing modern jumbo jets using the crash record of airplanes built in 1936. Of course, with the development of better drug treatments in psychiatry, the number of patients with persisting illness also decreased to the point that a psychosurgical operation is now warranted only for the very occasional patient, perhaps a few depressed patients in a thousand. But for that rare patient such as Edmund, the operation may be lifesaving. Unsuccessfully treated severe depression is a disease with a mortality rate similar to that of cancer. |
|
CAUSE AND EFFECT IN THE MENTAL DISORDERS isn’t a simple matter. Asking
why someone is depressed, for example, may be relevant if you’re dealing with depression
following a post-traumatic stress disorder, because it’s useful for planning treatment. But
what happened before an episode of manic-depressive illness may be quite irrelevant: the cause
lies elsewhere, at a different level of brain organization. “I was getting a little concerned, because we’ve been talking only about the organic psychiatric problems. I was about to ask you what in psychiatry isn’t organic?” A problem doesn’t have to be organic to be real. Organic just means damage that can be seen in the brain with current neuroanatomical techniques. Probably half or more of psychiatric problems surely aren’t organic, at least not at the beginning. Take the problem commonly seen in treating couples. Both husband and wife are undecided and somewhat ambivalent about having a child, or buying a house. One, for the sake of argument, will indirectly say, “Let’s do it.” And the other, mistrustful of making a decision just yet will, for a better defensive position, take the opposite stance rather than continuing to sit on the fence. This artificial creation of opposition, where both are really ambivalent, creates all sorts of trouble as positions harden and the problem festers. The undecided middle ground is where the doubts can be talked out. Going to extremes, however, has a certain amount of stability to it that maintaining the middle ground doesn’t. And so once you slip to extreme positions, it can be hard to get out. All it takes to fall into that trap is a normal brain. But the festering problem may have effects on the brain, just as it can elsewhere in the body. Stress reactions are bad for the stomach, leading to ulcers. And, because of the adrenal stress hormones stirred up, it’s bad for the brain in the long run. Stress may damage neurons in the hippocampus and set you up for memory problems later — converting a mild psychiatric problem into a rather different organic one. Both kinds of problems are “real” — and so are those in-between conditions that we have such difficulty labeling, the ones that look like neurological “hardware” problems but which we can’t yet see in the neuroanatomy. You don’t need to get wrapped up in the nomenclature difficulties to realize that psychotherapy can prevent more serious, expensive problems — such as broken homes. |
|
MANY OF THE ANXIETY PROBLEMS that psychiatrists treat are probably of that same stuck-in-a-rut nature. But not all. And a newly recognized disorder serves to show how one comes to
be recognized amid the psychiatric morass. Sometimes a psychiatrist, having been reminded of seizures or the behavioral tics of Tourette’s, will wonder if there is a subgroup of anxiety patients who really are different — the patients who say they have shortness of breath, break out in a sweat, tremble. Or maybe it’s flushes and chills accompanied by dizziness. And it happens for no good reason, just all of the sudden. Yet it lasts for as little as five minutes and seldom as long as a half hour — it’s not a fluctuating problem like most anxiety and most headaches. So it’s really an episodic thing, like seizures and tics, but involving autonomic symptoms. And then he remembers that these are things that the base of the frontal lobe might regulate. The psychiatrist asks herself, Could “panic attacks” be the medium-sized seizures of that part of brain? Or the petit mal of the more visceral parts of the thalamus? Or tics without the rest of Tourette’s? “Are they?” Ask next year. It’s another of your unfinished crossword puzzles. Certainly about ten percent of the population has suffered at least one panic attack. Two to three percent of women suffer from recurrent panic attacks, and maybe a half percent of men — they usually visit at least ten physicians before it gets properly diagnosed. Late twenties is the age when it usually develops. It often runs in families, being seen in about 20 percent of the patient’s first-degree relatives. Antidepressant drugs often help, although these patients usually aren’t depressed. And this same group of patients, it now turns out, are the ones who tend to suffer from fear of public places. About a third of panic attack victims also experience agoraphobia. “I bet they don’t want others to see them when they’re having a panic attack. I sure don’t want people to see me when I’m having a seizure.” I think you’re right. They’ve probably seen themselves in a mirror when having a panic attack, and know how they look to others. When they do go to a meeting or concert, they sit close to exits, so as to readily escape to a restroom where they can sit out the attack in privacy. They come to dislike situations that limit their flexibility, such as standing in a line or having to keep an appointment — especially getting their hair cut, where they’re trapped in a chair with someone working on them in a public place. Once you understand the panic attack problem, these particular fears of public places make perfect sense. There are patients with agoraphobia who don’t have panic attacks, but some of them are surely organic — maybe they have had a little right parietal stroke affecting their spatial orienting abilities, and so feel disoriented when they get away from familiar surroundings, worrying that they won’t be able to find their way home. So they refuse to travel without a companion, and hesitate to explore new places — all perfectly reasonable, once you understand the parietal lobe aspect, and quite different from the panic attack variety of agoraphobia. With an MRI brain image, the psychiatrist can often spot where the gray matter is missing. “So what about those people who are very shy?” asked Neil. “Kids seem to be born that way, while others are so bold as to worry their parents.” Maybe 15 percent of kids are at those shy-or-bold extremes as preschoolers, but it’s only several percent by the time they’re adults. And, of course, some people may become inhibited in dealing with the world because of some traumatic experience. What’s been surprising psychiatrists is that these personality disorders — which traditionally have been difficult to treat successfully — are responding to some of the newer drugs that selectively inhibit serotonin reuptake. It’s long been thought that those lawn-sprinkler systems for the monoamines might provide the bias that makes a person happy or sad, bold or shy, and so forth. But the downfall of those theories were that the earlier antidepressant drugs affected both norepi and serotonin — yet rarely affected “personality traits.” And the effect of some of the antidepressants isn’t simply to make people less shy. We’re still trying to figure it out. Psychiatrists get most of the leftover problems no other specialty can diagnose or treat, and so psychiatrists need a considerable tolerance for ambiguity and uncertainty, as well as a vast knowledge of medicine. But they’re on the frontier — occasionally they recognize some order amid all the individual variability and discover a new “neurological” disorder. INSTRUCTORS: You may create hypertext links to glossary items in THE CEREBRAL CODE if teaching from Chapters 6-8, e.g., <a href=http://www.williamcalvin.com/bk9gloss.html#postsynaptic>Postsynaptic</a> |
 Conversations with Neil's Brain:
Conversations with Neil's Brain: The Neural Nature of Thought and Language (Addison-Wesley, 1994), co-authored with my neurosurgeon colleague, George Ojemann. It's a tour of the human cerebral cortex, conducted from the operating room, and has been on the New Scientist bestseller list of science books. It is suitable for biology and cognitive neuroscience supplementary reading lists. ISBN 0-201-48337-8. | AVAILABILITY widespread (softcover, US$12).
|